Terminal Illness: Coping with Death and Dying. How do people cope with terminal illness? How do the reactions of dying children compare to those of dying adults? How can the responses of family members help or hurt the dying person? How can supportive care, such as that is given in hospice, help both the dying person and family members and friends?
Terminal Illness: Coping with Death and Dying.
How do people cope with terminal illness? How do the reactions of dying children compare to those of dying adults? How can the responses of family members help or hurt the dying person? How can supportive care, such as that is given in hospice, help both the dying person and family members and friends? The diagnosis of a terminal illness does not only affect the person carrying the illness but also family members, close friends, and even the health care providers who are providing services for them.
Terminal illness is something that happens unexpectedly, making it a non-normative event on the continuum of our lives. How people are able to cope when finding out they have a terminal illness is beyond me, which is why I picked this topic. In April, my family found out that my father is struggling with stage four head, neck and throat cancer, so if I were to compare the reactions of dying children to those of dying adults, for me it would equally as heart-rendering.
The responses of loved ones around them can either be very hopeful or harmful, in unfortunate events they are the ones struggling with the inability to cope, causing more stress in everyone’s life, and that is where I believe hospice comes in. Hospice is a “family affair”. There are two natural facts in life; we are all born, we all die. When you are faced with overwhelming situations and unquestionable loss, hospice is meant to help the surrounding loved ones understand, prepare for, and support each other through the tragedy of a terminal illness.
There are two natural facts in life; we are all born and we all die. When a patient is dying, for everyone involved patient, friends, family, sometimes even the health care providers, nothing is more emotionally draining than a terminal illness.
The difficulty that arises when it comes to answering “how” people cope with terminal illness is that everyone is different, so we can’t assume that one method of coping works for everyone. The briefing of Chapter 13 in
Adult Development and Aging
by Susan Krauss Whitbourne and Stacey B. Whitbourne provides three very helpful tips of learning how to cope and become more resilient. “1. Don’t let despair overwhelm you and don’t give into the temptation to give up and stop moving forward. 2. Tell yourself you can do it. Once you perceive that you can cope, you actually cope better. Positive “self-statements” can shore up your sense of self efficacy. 3.
View the loss as a test of faith, a sign that you can handle adversity, or at least a testament to your ability to see a silver lining in the ugliest circumstance.
Our trials are as much a part of our identities as are our successes” (Whitbourne, 2014, p. 261). The longer that you are alive to age and grow, the more battles you will have probably faced. We can be inspired by those who’ve lived longer than us and have survived all of the fortunes and misfortunes that life has tossed their way. From them, we can learn how to better get through our own experiences.
There are hardly any people in the world who are prepared to hear that they are living with a life-threatening illness, especially a child. When a child or adolescent is diagnosed with a terminal illness their whole world is flipped upside down in the blink of an eye, rather than focusing on going to school or hanging out with friends they are suddenly to cope with hospital stays or visits, countless tests, taking medicine, other possible treatments or surgeries, and above all, their illness that is unable to be cured or controlled.
In the research article “Teachers’ Knowledge and Support Systems Regarding Students with Terminal Illness” written by Kathryn W. Heller, Mari B. Coleman, Sherwood J. Best, and Judith Emerson, it is suggested and explained why it is difficult to conceptualize the death or terminal illness of a child, especially for the child.
The norms of society suggest that “children must be sheltered from the emotional impact of death and a belief that children cannot comprehend the meaning of death” (as cited in Holland, 2008; Heller, Coleman, Best, & Emerson, 2013, p. 5).
Child or adult, when someone close to us dies or becomes terminally ill it is one of the most devastating emotions that we may ever feel and sometimes, when facing death adults themselves may even feel helpless, making them incompetent to answer any questions a child may need answered in order to process their own emotions either for themselves or loved one who is dying or has been diagnosed with a terminal illness, leaving them lonely and confused.
Although this research states that when children reach the age of nine or ten understand the concept of death, they also include that “school-age children who are diagnosed with a terminal illness are often aware of the seriousness” (Heller, Coleman, Best, & Emerson, 2013, p. 6).
The concepts of death and reactions to death are both developmentally influenced by several variables other than age including: “intellectual function; the idea of death is abstract to a child and the ability of the child to comprehend death will parallel the child’s general cognitive development; culture, media exposure, religion, communication opportunities, and personal experiences” (Heller, Coleman, Best, & Emerson, 2013, p. 3).
The difference when it comes to adult’s versus child’s confrontation with terminal illness is that children are surprisingly able to achieve mindfulness much easier than adults can, making them surprisingly better at accepting the present moment, benefiting their ability to cope. In an article reviewing professional literature on death and dying:
counseling adults with terminal illness, Amie A. Manis and Nancy Bodenhorn believe that everyone “lives along a continuum of death anxiety and death awareness” (Manis & Bodenhorn, 2006, p. 2).
When children are raised and develop beliefs that death is a frightening and fearful experience and those children grow up to become adults it can be more difficult and take a little bit more time for them to be mindful and cope with untreatable illness.
Yalom, an existential psychiatrist provided us with observations on the numbers of ways older adults with terminal illness experience a “startling shift” that can’t be distinguished in any other way than “personal growth”, but I would suggest it’s a step towards mindfulness.
He carried on to list the shifts and changes which include: “a rearrangement of life’s priorities: trivializing of the trivial; a sense of liberation: being able to choose not to do the things that they do not wish to do; an enhanced sense of living in the immediate present; a vivid appreciation of the elemental facts of life: changing in the seasons, wind, falling leaves, the last Christmas, and so forth; deeper communication with loved ones;
fewer interpersonal fears, less concern about rejection, and a greater willingness to take risks” (Yalom, 1998, p. 190). When adults reach this “shift” they are further able to understand and possibly begin to manage personal coping mechanisms.
When individuals are coping with the terminal illness of a loved one they are presented with an extraordinary challenge that can also affect their mental health and well-being. Caring for someone who is close to dying becomes the primary focus of the caregiver and when they’re also a family member, managing the physical and psychological needs of not only the patient, but the family, including the caregiver, is especially important.
Terminal illness affects the lives of everyone involved; patients are compelled to give up their jobs, the caregiver (usually the spouse or child) is also forced to change work habits, miss school, and even sell assets to afford healthcare. Grieving a family member can also include a variety of psychological issues such as:
despair, anxiety, anger, loneliness, agitation, fatigue, crying, withdrawal, low self-esteem, preoccupation with thoughts of the person who is dying, problems with memory and concentration, helplessness and hopelessness, and sleep disturbance (Waldrop, 2007).
All of these built up emotions while watching someone you love slowly die is a lot for one person to handle and that’s why hospice is so important for both the patient and family members. The purpose of hospice is to “enhance the quality of life of the, focus on comfort rather than cure, provide support to the entire family through an interdisciplinary team
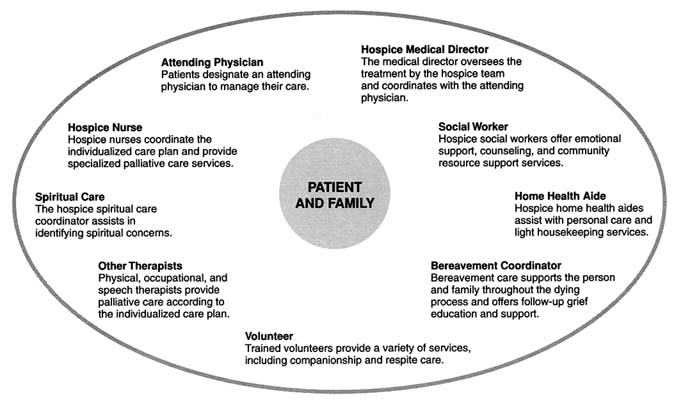
(e.g., nurse, social worker, physician, chaplain, nursing assistant), and deliver hospice services in the patient’s environment” (Wolfe, Hinds, & Sourkes, 2011). Even when faced with a terminal illness it is still possible for patients and families to adapt and continue living their lives. In Albom’s (1997)
Tuesdays With Morrie
he noted “when you realize you are going to die, you see everything much differently… Learn how to die and you learn how to live” (Albom, 1997, p. 83).

References
- Heller, K. W., Coleman, M. B., Best, S. J., & Emerson, J. (2014). Teacher’s knowledge and support systems regarding students with terminal illness. Physical Disabilities: Educational & Related Services, 16 (6), 1-10. Retrieved from https://eds-a-ebscohost-com.proxy-calu.klnpa.org/eds/detail/detail?vid=3&sid=a74f077e-7b5c-4981-85b1-ecfde5bba5c7@sessionmgr4006&bdata=JnNpdGU9ZWRzLWxpdmUmc2NvcGU9c2l0ZQ==#db=eric&AN=EJ749739.
- Holland, J. (2008). How schools can support children who experience loss and death. British Journal of Guidance and Counseling, 36(4), 411–424.
- Manis, A. A., & Bodenhorn, N. (2006). Preparation for counseling adults with terminal illness: Personal and professional parallels. Counseling and Values. 50 (3), 2. Retrieved from https://eds-a-ebscohost-com.proxy-calu.klnpa.org/eds/detail/detail?vid=3&sid=a74f077e-7b5c-4981-85b1-ecfde5bba5c7@sessionmgr4006&bdata=JnNpdGU9ZWRzLWxpdmUmc2NvcGU9c2l0ZQ==#db=eric&AN=EJ749739.
- Albom, M. (1997). Tuesdays with Morrie: An old man, a young man, and his greatest lesson. New York, NY: Doubleday.
- Yalom, I. D. (1998). Existential psychotherapy. In B. Yalom (Ed.), The Yalom reader: Selections from the work of a master therapist and storyteller (pp. 167-265). New York: BasicBoo
- Waldrop, D. (2007). Caregiver grief in terminal illness and bereavement: A mixed-methods study. Health & Social Work, 32 (3), 197-206. Retrieved from https://eds-a-ebscohost-com.proxy-calu.klnpa.org/eds/detail/detail?vid=2&sid=7269e6e9-23af-4410-b144-5639c0c90528@sdc-v-sessmgr03&bdata=JnNpdGU9ZWRzLWxpdmUmc2NvcGU9c2l0ZQ==#AN=106174495&db=ccm.
- Whitbourne, S. K., & Whitbourne, S. B. (2014). Adult development & aging: Biopsychosocial perspectives. Hoboken, NJ: John Wiley & Sons.
- Wolfe, J., Hinds, P., & Sourkes, B. (2011). The language of pediatric palliative care. In J. Wolfe, P. Hinds, & B. Sourkes (Eds.), Textbook of interdisciplinary pediatric palliative care (pp. 3–6). Philadelphia: Elsevier.
Read More On:
- Reflective practice is an integral part of developing skills to improve
- Impact of Medical Marijuana on School Nursing and the School Nurse
- Causes and Solutions to Global Nursing Shortage.
- Medical Marijuana Treatment for Parkinson’s Disease
- The Health Inequalities Between Genders
Do not hesitate to contact our professionals if you need help with your essay even after going through our example guide.