The Health Inequalities Between Genders. Gender norms and values are not fixed. They evolve over time, vary substantially from place to place, and are subject to change. Thus, the poor health consequences resulting from gender differences and gender inequalities are not static either. If you need assistance with writing your nursing literature review, our professional nursing literature review writing service is here to help!
The Health Inequalities Between Genders.
Gender norms and values are not fixed. They evolve over time, vary substantially from place to place, and are subject to change. Thus, the poor health consequences resulting from gender differences and gender inequalities are not static either. They can be changed” (The WHO, 2010). To understand health inequalities that exist between men and women we need to appreciate gender inequalities Materialist theories explain gender inequality as an outcome of how women and men are tied to the economic structure of society.
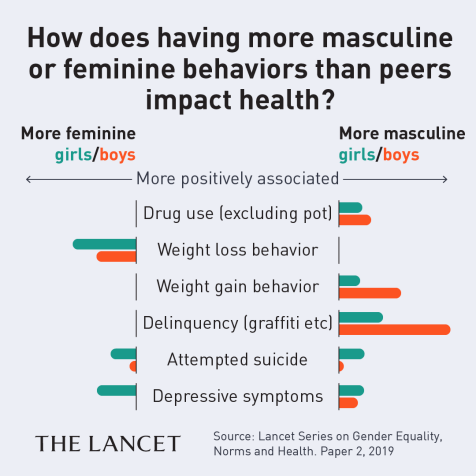
Such theories stress control and distribution of valued resources as crucial facts in producing stratification thus allowing us to understand why health inequalities between men and women exist and how they are dealt with differently by the two sexes. It has become increasingly widely accepted that ‘women get sicker but men die quicker’, based on research on gender and health from the 1970s, this is an oversimplification. This essay will look at the health inequalities that exist between men and women.
It was determined that 51.7% of females and 21.3% of males were exposed to negative gender discrimination (Keskinoglu, P et al. 2007). Changes have been made within the spheres of society that indicate women are more included, however they are still left to strive for equalities with men in different fields. One such area is health. Gender identities determine social strata’s that create and restrict illness and how it is experienced.
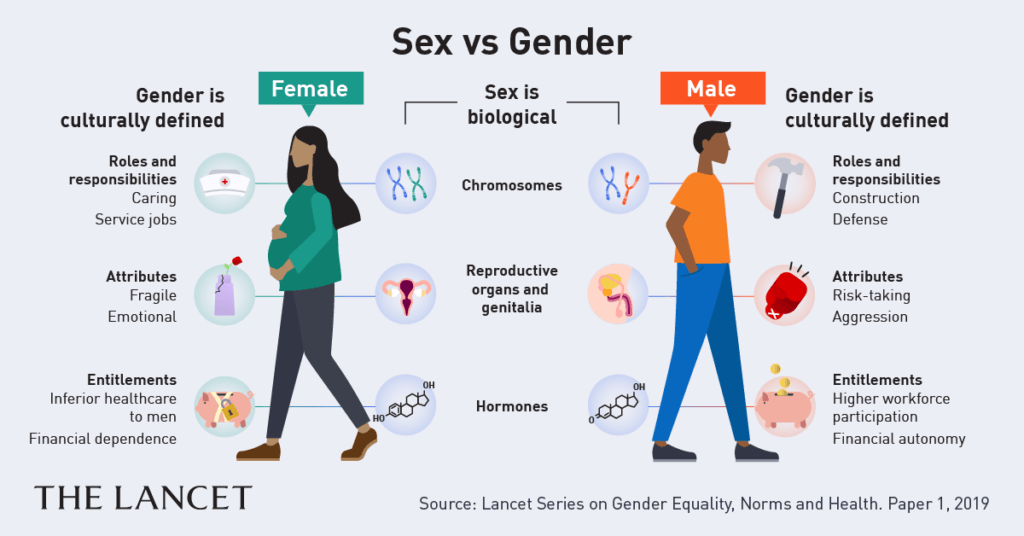
Gender and sex need to be understood allowing us to appreciate how biological and sociological factors contribute to health inequalities amongst men and women. Gender refers to ‘socially created characteristics of men and women whilst sex refers to the biological differences between men and women’ (Letherby, G. 2005). Factors such as Biological, social, cultural and economical show variance on the impact they have on men and women, they are seen to contribute to the differences that exist.
Biological Differences
Biological factors in human health, including reproductive, hormonal differences and genetic influences, have been known for some time. However, the full impacts of these factors on health are only now being understood. Differences in the health of women and men reflecting reproductive variations are perhaps the most apparent.
Women’s health is affected by their capacity to conceive, not only in terms of the consequences for their health of pregnancy and childbirth, but also because they are at risk of disorders associated with reproductive organs -cancer of the ovary or breast, for example, or infections of the reproductive tract. Men, on the other hand, are at risk of conditions specifically associated with male reproductive organs testicular cancer, prostate cancer, or an enlarged prostate gland. (Payne, 2006.)
More attention has been paid to biological differences by the health services and sometimes more in the favour of women. Specialised services are available to women. They focus on needs mentioned above. This was reflected in figures which showed a 82% increase in birth at hospital from 1927 to 1997 (Lloyd & Woroch 2000: Scambler, A. 2003) including the average rate of caesarean sections that rose from under 10% in 1970s to 17% by 1997 (Scambler, A. 2003). Furthermore the increase in breast cancer diagnosis has been associated with better screening procedures for women.
Statistics from 1998 showed that within the previous 5 years 84% of women aged 25-64 in England had been screened at least once for breast cancer, this in comparison to the 44% in 1988 when national screening first began (Scambler, A. 2003). Survival rates in association with breast cancer have shown a improvement with 70% of cases showing successful recovery due to effective improvements in treatments (1CRF 2001: Scambler, A. 2003).
Comparing these findings to those for men’s reproductive biology very little progression has been made. Statistics show a 69% increase in prostate cancer mortality between 1971 and 2005 (Cancer Research UK. 2007). Men are less likely than women to carry out self-examinations; they are less likely to examine themselves for prostate or testicular cancer than women are to conduct breast self-exams (Courtenay, 2000).
Gender Roles
Research by Emslie et al. (1999), suggests that health differences between men and women, particularly those associated with minor morbidity, are strongly associated with occupational and socio-economic inequalities. Differences in health across the life course and the risk of poor health in later years reflect the cumulative effects of socio-economic disadvantage, including paid work, over a lifetime (Macintyre et al., 1996).
Women are more likely to work in occupations which are low-paid, have few benefits and offer less in terms of self-esteem. These factors contribute to explanations of differences between women and men in mental and psychological well-being in particular (Pugliesi, 1999). Health variations can be explained in the context of gender expectations. The dual roles of women the family based roles and the paid work have shown gender differences in exposure to stress. Women have always been regarded as the major providers of care within the home.
It is presumed that caring generally is a women’s job. Increased contribution of unpaid carers at home includes women. In most cases they prioritize the needs of the family at the expense of their own health (Leatherby, G. 2005). The home being a refuge for women means that victims of domestic violence will remain in undesired surrounding for the purpose of fulfilling their roles as wife’s or mothers. World Health Organization figures suggest that between 20-30% prevalence is in western countries with other countries having rates as high as 52% (Scambler, A. 2003).
Abuse experienced can be in different forms such as physical, emotional, psychological and sexual and in majority of the cases is directed towards females by males. Brisson suggested in (1999), ‘while tension raises the blood pressure of both sexes during the day, working mothers remained stressed for longer into the evening, increasing the danger of heart disease and strokes’ (Scrambler, A. 2003). A study by the office of National Statistics (1997) showed that unpaid work performed out ‘love’ when valued as paid employment would have amounted to £739 billion/annum (Scambler, A. 2003). Figures for pay obtained in 2002, despite the equal pay act 1970 indicated a 20% pay gap between men and women.
Women are twice as likely in comparison to men to be exposed to jobs that don’t provide higher health insurance, health screening and other forms of welfare such as sports club (Scambler, A. 2003). In the labour market in respect of gender women remain compromised due to physical and mental health consequences due to stress, low levels of social, personal and material resources (McDonough, P and Walaters, V. 2001)
Morbidity
The idea that women are sicker than men has been supported by large morbidity rates amongst females. This results in a reduced quality of life experienced by women over their life time (McDonough, P and Walters, V .2001). Research indicates that implications of psychological and physical behaviour from violent men contributed greatly to high morbidity rates of women and the use of health care (Bird, C and Riecker, P. 1999). Evidence suggests that women use healthcare services more than men.
With this concept it may be probable that genuine health problems are associated with stereotypical views of women being sensitive and health problems passed off as feminine notions. Research has shown that women are far more likely to be prescribed psychoactive drugs in comparison to men, in some instances the figures have been double that of the men (Scambler, A. 2003). When men experience mental health problems they are treated more seriously in comparison to women.
Traditional masculine portrayals of men as mentally robust means they’re not as likely to get see a doctor unless it’s genuinely serious. Payne (2001) and Prior (1999) discussed how men are passed easily through the primary care filter in comparison to women who are more likely to get the treatment from GPs (Scambler, A. 2003). The way in which men and women with the same medical condition are treated is a broad area of research. In the US, Men are more likely to receive a kidney transplant in comparison to women (Letherby, G.2005).
Furthermore, the main cause of death of women and men over 75 is CHD and stroke, however targets set to eliminate these conditions were for individuals under 65 (Letherby, G.2005). This exclusion was shown to affect women that were older than men. This was supported further by data from Office of National Statistics (1996) which showed that were 50%more women aged 65 and over in comparison to men (Letherby, G. 2005). This shows that occlusion of older people from areas such as clinical research; procedures and treatment are seen to affect women far more than they do men.
Mortality
Men have higher mortality rates in comparison to women this correlation can found globally. High mortality rates can be a result of factors such as heavy drinking, smoking and participating high risk activities. Men are also exposed to more hazards in their jobs (Waldron, I. 1983). Lung cancer due to cigarette smoking is the second common cancer amongst men with 22,000 new cases being diagnosed yearly (Cancer Research UK. 2008). It has been suggested that men cope with stressful situations by diverting their attention from the stress through heavy drinking.
Office for National Statistics (2008) stated that 31% of men drink more than 21 units/week and 8% drink more than 50 units/week. The recommended amount is 12units/week by the government. (Cancer Research UK.2008). Increase in unemployment, loss of direction and lack of positive role models leading to a low self worth and insecurity is believed to be a key contributor to increased suicidal rates in young men. Research shows that between the ages of 15-24 suicide rates have increased by two and a half times and in those aged 25-44 they have doubled (Scambler, A.2003).
High rates of male mortality have been contributed by occupations that involve direct risk to life such as soldiers, policemen and participation in dangerous sports. Masculinity is seems needs to be confirmed via risk-taking behaviours. It has been suggested that the number of young men killed in accidents explains the excess mortality amongst 15-25’s (Scambler, A. 2003). It has been suggested that women are more likely to outlive a spouse, become single parents and become sole carers of elderly relatives. This leads to women facing economic hardship at a higher scale. Strains of such kind can have both direct and indirect implications on the health of women (Bird, C and Riecker, P. 1999).
Ethnicity
(Ahmed et al., 2003; Phillips and Brooks, 1998; Chapple et al., 1998; Vandenbrinkmuinen et al, 1994) suggested that women from South Asian ethnic groups would prefer to see a female physician especially with intimate issues to do with reproduction. The sex of the physician can determine ethnic women seeking healthcare. In regards to men’s preferences for female or male doctors, they are less likely to show a preference, and when they do in consultations which involve physical examinations, they often prefer a female doctor (Fidler et al, 2000).
(Ahmed et al. 2003) found that Bangladeshi women use more self-care, unqualified practitioners, and unlicensed medicines compared to men who use the formal systems of care. Social and cultural constraints make access to medicine and services more difficult for women. (Baghadi, 2005) found that permission from male members of family would need to be sought. (Tanner and Vlassoff, 1998) found that women in some countries were unable to travel alone on public transport, if no one is able accompany them, they can’t attend health appointments.
Conclusion
For us to understand the prevalence of health differences amongst men and women we need to understand social and biological factors. Sex and gender interact with differences such as, social class, ethnicity and sexuality, these affect the health of women and men. This can be due to a health disadvantage in one sex arising as a result of biological differences in men and women or even due to social circumstances or both combined.
Women for example should be treated appropriately for stress management, addressing both medical and social issues. Assumptions that sex differences or social factors are the sole contributors to the status of health can have serious implications such as preventing research into better treatments and advancements that could benefit both sexes.
Gender and sex differences are important when addressing health inequalities. A gender stereotype that influences the needs of the sexes can be detrimental to the quality of health care. For example, In men the failure to recognise health risks associated with fertility and in women underestimating cardiovascular disease resulting in inequitable treatment medically and failure of recognition results in poor understanding of health behaviours.
Social identity, resources available and opportunities determine health and well-being. In order to reduce health inequalities and improve health amongst men and women it’s important to adapt an interdisciplinary strategy which will allow us to understand the real implications associated with gender and health.
Read More On:
- Psychological and Sociological Factors Influencing Patient Care
- Critical Care of Chronic Obstructive Pulmonary Disease Patient: Reflection paper.
- Knowledge and Skills Hand Hygiene: Reflective Essay
- Levines Conservation Model Theory: Case Study.
- Depression Intervention for Older Adults.
Do not hesitate to contact our professionals if you need help with your essay even after going through our example guide.