This article is an essay about the use of dabigatran and aspirin in the prevention of stroke. Study it to learn how to write similar essays and follow it to gain insights into how you can get expert essay writing help.
The Use of Dabigatran and Aspirin in Stroke Prevention
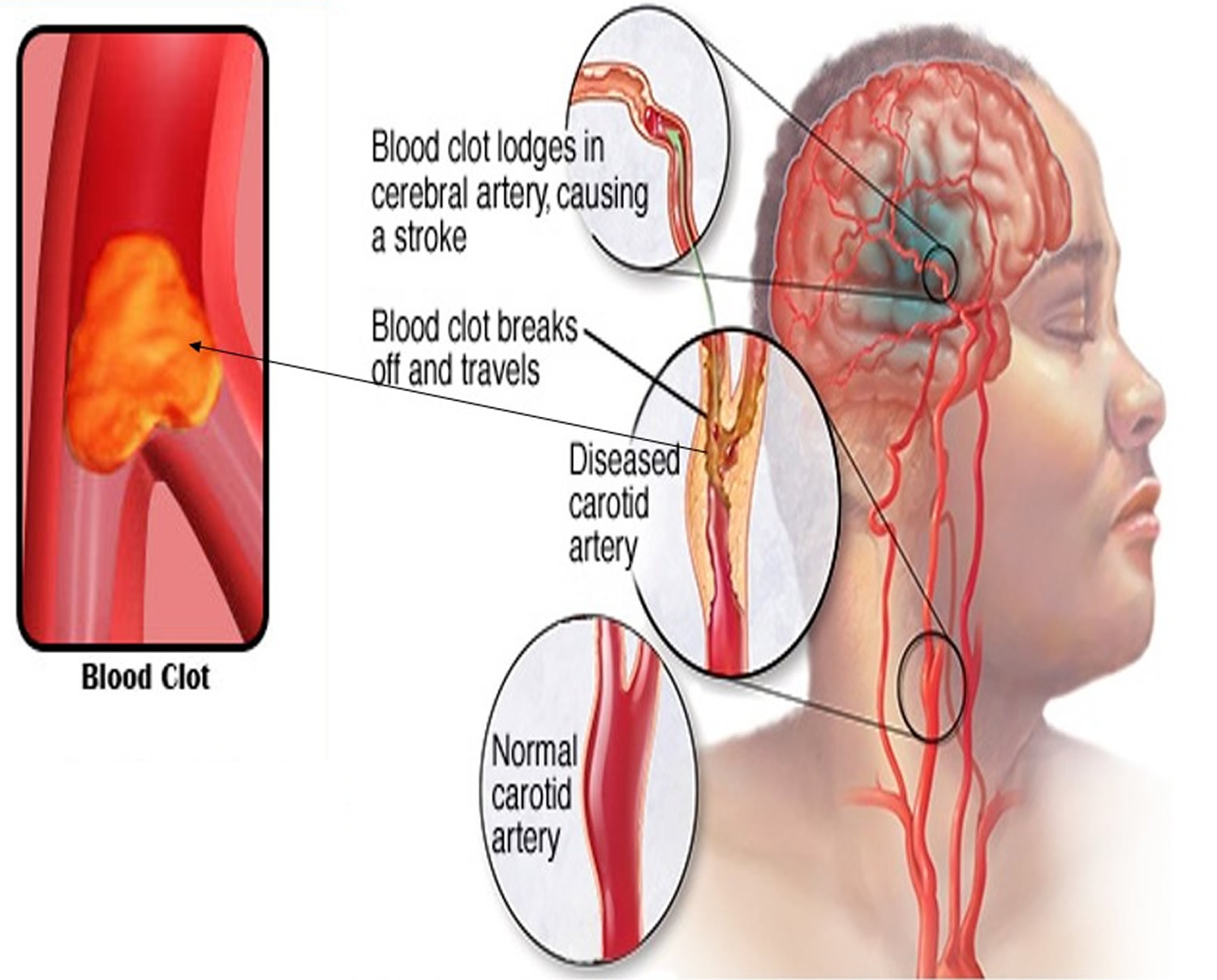
Embolic stroke, a type of ischemic stroke, occurs when a vessel in the brain is blocked. Brain tissue is deprived of oxygen and can die in just a few minutes. Thrombotic issues like blood clots contribute to this kind of stroke which constitutes 87% of all strokes. An embolic stroke occurs when a thrombus travels from another part of the body (embolism) and becomes lodged in a vessel in the brain (Johns Hopkins Medicine, 2019).
Those at increased risk for thrombosis that may lead to stroke include smokers, those with atherosclerosis, and diabetes, who are obese or have metabolic syndrome. Heart failure or an irregular heartbeat called atrial fibrillation (afib) may also contribute to the development of clots in the heart that may be released into circulation, ultimately reaching the brain (American Heart Association, 2019)
Overview of Current Stroke Therapy
If a stroke is occurring, there is only one medication FDA-approved for the treatment, tissue plasminogen activator (tPA). This drug works by dissolving the clot to stop the ischemic damage to the brain (National Stroke Association, 2019) It is best if the medication is given within 4 hours and there could be sustained damage to the tissue leaving the patient with deficits. For this reason, primary treatment is focused on prevention.
Historically, therapy for stroke prevention centered on the administration of aspirin or warfarin to prevent the formation of clots. The Trial of Org 10172 in Acute Stroke Treatment (TOAST) developed in the 1990s further clarified appropriate treatment by classifying types of ischemic strokes. Following this, the implementation of clopidogrel into treatment regimens provided more options. Unfortunately, these medications proved to have negative effects in studies due to the tendency to cause hemorrhage, though when used in those with low bleeding risk, the results were satisfactory (Gurol & Kim, 2018).
In recent years, studies have proven that the use of non-vitamin K antagonist oral anticoagulants (NOACs) outperforms warfarin in nonvalvular afib trials. The first NOAC approved for use in 2010 was dabigatran (Pradaxa) which is classified as a direct thrombin inhibitor. Three more NOACs are now available: rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa), and are classified as factor Xa inhibitors (Cruz & Summers, 2016). More data is being collected and recommendations for use are making these medications a first-line treatment for many providers (Gurol & Kim, 2018).
NOACs such as dabigatran have been proven more effective than warfarin in the RE-LY (Randomized Evaluation of Long-term Anticoagulation) trials for the prevention of nonvalvular afib (Edmunds & Mayhew, 2014). This study will examine how dabigatran performs compared to aspirin in the prevention of stroke. Current guidelines for the treatment of this kind of ischemic stroke call for aspirin, dipyridamole ER and aspirin, or clopidogrel and aspirin (Diener, et al., 2019)
Analysis of the Study
In the study entitled, Dabigatran for Prevention of Stroke after Embolic Stroke of Undetermined Source, researchers compare the effectiveness of dabigatran versus aspirin for the prevention of stroke. Previous research indicates rivaroxaban was no more effective than aspirin, but studies have not included dabigatran (Diener, et al., 2019).
At 564 different sites in 42 countries, 5,390 participants were randomly selected for this trial. The selected participants were divided in half: 2,695 received aspirin 100mg once daily and 2,695 received dabigatran 150mg once daily or 110mg twice daily. Dabigatran dosage was decided based on age greater than 75 years and/or creatinine clearance of 30-50 mL/min received the twice a day dosing. All participants were greater than 60 years of age and the mean age was 64.2 years old.
Participants had all experienced an embolic stroke of an undetermined source in the previous months or had risk factors present. Baseline characteristics of participants, including comorbidities, gender and race are detailed in table 1 appendix A. Efficacy was based on the prevention of occurrence of stroke after treatment. The study design was a randomized double-blind trial conducted between December 2014 and January 2018 concluding with a median follow up at 19 months. Appropriate approval by ethics committees at all locations was secured (Diener, et al., 2019).
All outcomes were discussed in a time-to-event analysis and included the following: ischemic stroke, non-fatal myocardial infarction (MI), and death from cardiovascular causes. A modified Rankin scale was used to display data for disabling recurrent stroke. Results on the Rankin scale ranged from 0-6 with 0 being no deficit and 6 being death. Type I errors were eliminated through adjustments to statistical significance (Diener, et al., 2019).
In the dabigatran group, 177 participants had a recurrent stroke of any kind compared to 207 in the aspirin group. 172 and 203 strokes respectively were deemed ischemic in nature. Dabigatran was discontinued at 19 months in 671 participants and aspirin in 568, both due to adverse events as the main reason. The composite outcome for combined nonfatal stroke, MI, or cardiovascular death was 207 participants in the dabigatran group and 232 in the aspirin group. Nonmajor bleeding occurred in 70 participants and 41 participants, respectively (Diener, et al., 2019).
Ultimately, dabigatran did not prevent recurrent stroke more effectively than the aspirin regimen. While major bleeding was not greater with dabigatran, there was more nonmajor bleeding events in the dabigatran group (Diener, et al., 2019). These results in addition to the increased cost of dabigatran should be considered when designing a treatment regimen.
This study’s strengths were a large study size and good generalizability. The number of recurrent strokes was not outside the margin of prediction. Weaknesses include the ad hoc nature of the test and the inability to determine if dabigatran was more effective for those with undiagnosed afib (Diener, et al., 2019).
New Findings and Current Therapy
Although dabigatran does not outperform aspirin in trial studies, it is as effective. When prescribing medication, the provider must consider many factors, including what risk factors the patient may have, especially the risk of bleeding. Determining the cause of a previous stroke or the risk factors present that may induce stroke, is the first, and most critical determination for treatment. Once this has been decided, medication can be selected to address the underlying cause. NOACs such as dabigatran are relevant in the treatment and prevention of ischemic stroke and provide options that were not previously available.
A Case Study
Advanced Pharmacology Spring 2019 presents the following case study in week three:
CC/HPI
TG is 57-year-old male who presents to your office with complaints of frequent nosebleeds (3 in the past week) and easy bruising. He also complains that he has a cold. TG has a history of chronic atrial fibrillation for which he takes warfarin. About 2 weeks ago he started taking cimetidine (Tagamet) OTC for symptoms of heartburn.
Medications:
Warfarin 7mg QD
Digoxin 0.25mg QD
Cimetidine OTC BID
Pseudoephedrine SR 120mg BID
Allergies: NKDA
Physical Examination:
GEN: Well developed, well-nourished man
VS: BP 175/96, HR 70, irregularly irregular, RR 18, Wt. 94kg
HEENT: WNL
COR: slight atrial enlargement
CHEST: WNL
ABD: (+) bowel sounds
EXT: bruising on arms and knees
NEURO: A&O x 3
ECG: a. fib
Laboratory
Na 143
K 4.5
Cl 99
CO2 25
BUN 18
SCr 0.9
INR 4.7
Hct 43
Hgb 14
Digoxin 1.6ng/ml (Lynch, 2019)

This patient is taking warfarin (Coumadin) to prevent clot formation related to his afib. Embolism of these clots could cause ischemic stroke, as discussed previously. He has a supratherapeutic INR of 4.7. In cases of nonvalvular afib, cases of afib not caused by valve failure, NOACs offer another option of treatment. Coumadin is extensively protein bound causing competition with other medications that are protein bound creating chances for drug to drug interactions or increased serum levels (Condo, 2018).
In addition to this, Coumadin requires frequent monitoring to ensure therapeutic INR. In contrast, using an oral direct thrombin inhibitor such as dabigatran (Pradaxa) requires no monitoring and has much fewer drug interactions. Dabigatran does not have any significant interaction with any of the medications that this patient is taking. Of course, it should be recommended that the patient not take pseudoephedrine with digoxin due to the potential for arrhythmia (Epocrates; Athena Health, 2019).
It is important to teach the patient that dabigatran should be stored in an airtight, original container and discarded 30 days after opening. Most patients are started on 150mg twice daily. It is essential for a patient to adhere to the treatment regimen to avoid the potential for the occurrence of the black box warning associated with dabigatran, the development of stroke, or the thrombotic event.
Before transitioning this patient to dabigatran, the patient’s INR should be decreased to <2. This can be accomplished by the administration of vitamin K. Should it be required, the reversal agent for dabigatran is idarucizumab (Praxbind) (Condo, 2018). Adverse reactions in addition to stroke or thrombosis if suddenly discontinued include, GI bleeding, bleeding, thrombocytopenia, hypersensitivity, or anaphylaxis (Epocrates; Athena Health, 2019). Follow up should occur with this patient in two weeks to ensure that no adverse reactions have occurred.
This case differs from the study as dabigatran is being used to replace warfarin, which studies like RE-LY have supported. As dabigatran does not perform better than aspirin, and aspirin lacks the interactions and required monitoring of warfarin, it would not be prudent to switch a patient from aspirin for thrombosis prevention to dabigatran without clear reason. If it was determined that dabigatran was a more appropriate therapeutic regimen, the same adverse reactions discussed above would be included in patient education and monitoring.
Therefore, this exercise further concludes that the selection of mediation for the prevention of clot formation and subsequent potential ischemic stroke is a very individualized process that begins with determining the risk factors involved, comorbidities, potential adverse effects, cost of medication, and required monitoring. Being knowledgeable of all medications and their therapeutic properties allows providers to select the medication that best meets the client’s needs.
Appendix A
 (Diener, et al., 2019)
(Diener, et al., 2019)
References
- American Heart Association. (2019). Understand Your Risk of Blood Clotting. Retrieved from American Heart Association: Heart attack and Stroke Symptoms: https://www.heart.org/en/health-topics/venous-thromboembolism/understand-your-risk-for-excessive-blood-clotting
- Condo, K. (2018). Advanced Pharmacology PYC 612 Supplemental Material Document . Retrieved from Indiana Wesleyan University: file:///C:/Users/eem31/Desktop/Adv%20Pharm/Supplemental%20Guide%20for%20Adv%20Pharm.pdf
- Cruz, J., & Summers, K. (2016). Novel Oral Anticoagulants. Pharmacy Times .
- Diener, H., Sacco, R., Easton, J., Granger, C., Bernstein, R., Uchiyana, S., . . . Odinak, M. (2019). Dabigatran for Prevention of Stroke after Embolic Stroke of Undetermined Source. New England Journal of Medicine, 1906-1917.
- Edmunds, M., & Mayhew, M. (2014). Pharmacology: for the primary care provider . St. Louis: Elsevier.
- Epocrates; Athena Health. (2019). Drug Look-up . Retrieved from Epocrates: https://online.epocrates.com/drugs
- Gurol, M. E., & Kim, J. (2018). Advances in Stroke Prevention in 2018. Journal of Stroke, 143-144.
- Johns Hopkins Medicine. (2019). Types of stroke. Retrieved from Johns Hopkins Medicine: https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/types-of-stroke
- Lynch, K. (2019). Advanced Pharmacology. Retrieved from Indiana Wesleyan Bright Space: https://brightspace.indwes.edu/d2l/le/content/71782/viewContent/1164334/View
- National Stroke Association. (2019). Stroke Treatments. Retrieved from National Stroke Association: https://www.stroke.org/we-can-help/survivors/just-experienced-stroke/stroke-treatments/
Read More On
- What is combined pulmonary fibrosis and emphysema?
- Why is reflection important in mental health nursing?
- Evidence-Based Practice requirements that all healthcare professionals need to understand.
- HIV/AIDS effects on the population and the factors contributing to its spread
- Why is Brazilian But Lift a dangerous cosmetic surgery?
Do not hesitate to contact our professionals if you need help with a similar article.