This article is an essay about blood pressure and hypertension. Study it to learn how to write similar essays and follow it to gain insights into how you can get expert essay writing help.
Blood Pressure and Hypertension
Definition of Hypertension and Blood Pressure
‘Hypertension is a common and major cause of stroke and other cardiovascular diseases. There are many causes of hypertension, including defined hormonal and genetic syndromes, renal disease, and multifactorial racial and familial factors. It is one of the leading causes of morbidity and mortality in the world and will increase in worldwide importance as a public health problem by 2020 (Murray and Lopez 1997).
Blood pressure (BP) is defined as the amount of pressure exerted when the heart contract against the resistance on the arterial walls of the blood vessels. In clinical terms high BP is known as hypertension. Hypertension is defined as sustained diastolic BP greater than 90 mmHg or sustained systolic BP greater than 140 mmHg. The maximum arterial pressure during contraction of the left ventricle of the heart is called systolic BP and minimum arterial pressure during relaxation and dilation of the ventricle of the heart when the ventricles fill with blood is known as diastolic BP (Guyton and Hall 2006).
Categories of Hypertension
Hypertension is commonly divided into two categories; primary and secondary hypertension. Primary hypertension, often called essential hypertension is characterized by a chronic elevation in blood pressure that occurs without the elevation of BP pressure resulting from some other disorder, such as kidney disease. Essential hypertension is a heterogeneous disorder, with different patients having different causal factors that lead to high BP.
Essential hypertension needs to be separated into various syndromes because the causes of high BP in most patients presently classified as having essential hypertension can be recognized (Carretero and Oparil 2000). Approximately 95% of hypertensive patients have essential hypertension. Although only about 5 to 10% of hypertension cases are thought to result from secondary causes, hypertension is so common that secondary hypertension probably will be encountered frequently by the primary care practitioner (Beevers and MacGregor 1995).
In normal mechanism when the arterial BP raises it stretches baroceptors, (that are located in the carotid sinuses, aortic arch, and large artery of the neck and thorax) which send a rapid impulse to the vasomotor center that resulting in vasodilatation of arterioles and veins which contribute in reducing BP (Guyton and Hall 2006). Most of the books suggested that there is a debate regarding the pathophysiology of hypertension.
Factors that Contribute to Increased Blood Pressure
A number of predisposing factors that contribute to increased BP are obesity, insulin resistance, high alcohol intake, high salt intake, aging and perhaps sedentary lifestyle, stress, low potassium intake, and low calcium intake. Furthermore, many of these factors are additive, such as obesity and alcohol intake (Sever and Poulter 1989).
Pathophysiology of Hypertension
The pathophysiology of hypertension is categorized mainly into cardiac output and peripheral vascular resistance, renin-angiotensin system, autonomic nervous system, and other factors. Normal BP is determined and maintained the balance between cardiac output and peripheral resistance. Considering essential hypertension, peripheral resistance will rise in normal cardiac output because the peripheral resistance depends upon the thickness of the wall of the artery and capillaries and the contraction of smooth muscle cells which is responsible for increasing intracellular calcium concentration (Kaplan 1998).
In the renin-angiotensin mechanism, the endocrine system plays important role in maintaining blood pressure; especially the juxtaglomerular cells of the kidney secrete renin in order to respond to glomerular hypo-perfusion. And also renin is released by the stimulation of the sympathetic nervous system which is later converted to angiotensin I then again it converts to angiotensin II in the lungs by the effect of the angiotensin-converting enzyme (ACE). Angiotensin II is a potent vasoconstrictor and also released aldosterone from the zona glomerulosa of the adrenal gland which is responsible for sodium and water retention.
In this way, the renin-angiotensin system increases the BP (Beevers et al 2001). Similarly, in the autonomic nervous system, the sympathetic nervous system plays a role in the pathophysiology of hypertension and key to maintaining normal BP as it constricts and dilates the arteriolar. The autonomic nervous system considers important in short-term changes in BP in response to stress and physical exercise. This system works together with the renin-angiotensin system including circulating sodium volume.
Although adrenaline and nor-adrenaline don’t play an important role in causes of hypertension, the drugs used for the treatment of hypertension block the sympathetic nervous system which had played a proper therapeutic role (Beevers et al 2001). Other pathophysiology includes many vasoactive substances which is responsible for maintaining normal BP. They are enothelin bradikinin, endothelial derived relaxant factor; atrial natriuretic peptide, and hypercoagulability of blood are all responsible in some way to maintain BP (Lip G YH 2003).
The seventh report of the Joint National Committee (JNC-VII) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure defines some important goals for the evaluation of the patient with elevated BP which are detection and confirmation of hypertension; detection of target organ disease (e.g. renal damage, congestive heart failure); identification of other risk factors for cardiovascular disorders (e.g. diabetes mellitus, hyperlipidemia) and detection of secondary causes of hypertension (Chobanian et al 2003).
Pharmacological and Non-Pharmacological Treatment of Hypertension
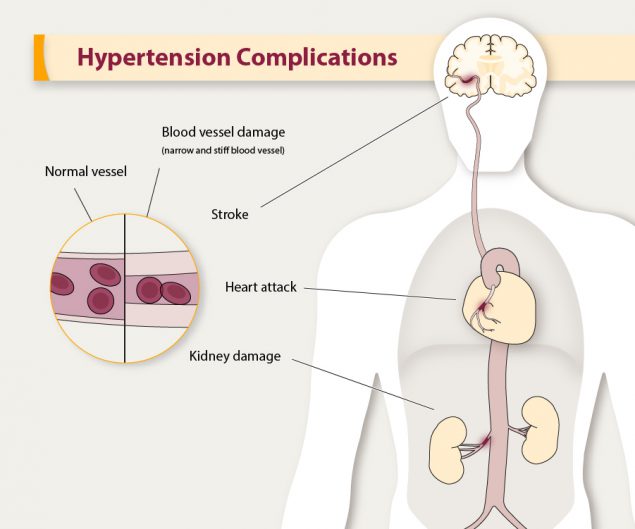
Most hypertensive patients remain asymptomatic until complications arise. Potential complications include stroke, myocardial infarction, heart failure, aortic aneurysm and dissection, renal damage, and retinopathy (Zamani et al 2007). The drug selection for the pharmacologic treatment of hypertension would depend on the individual degree of elevation of BP and contradictions. Treatment of non-pharmacologic hypertension includes life-style, weight reduction, exercise, sodium, potassium, stopping smoking and alcohol, relaxation therapy, and dietary improvements, followed by pharmacology therapy.
Commonly used antihypertensive drugs include thiazide diuretics, β-blockers, ACE inhibitors, angiotensin receptor blockers, calcium channel blockers, direct vasodilators and α-receptor antagonists. Diuretics have been used for decades to treat hypertension and are recommended as first-line therapy by JNC-VII guidelines after antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT) success. They reduce circulatory volume, cardiac output, and mean arterial pressure and are most effective in patients with mild-to- moderate hypertension who have normal renal function.
Thiazide diuretics (e.g. hydrochlorothiazide) and potassium sparing diuretics (e.g. spironolactone) promote Na+ and Cl- excretion in the nephrone. Loop diuretics (e.g. furosemide) are generally too potent and their actions too short-lived, however, they are useful in lowering blood pressure in patients with renal insufficiency, who often do not respond to other diuretics. Diuretics may result in adverse metabolic side effects, including elevation of creatinine; glucose, cholesterol, triglyceride levels, hypokalemia, hyperuricemia, and decreased sexual function are potential side effects. The best BP lowering response is seen from low doses of Thiazide diuretics (Kaplan 1998).
Β-blocker such as propranolol are believed to lower BP through several mechanisms, including reducing cardiac output through a decreased heart rate and a mild decrease in contractility and decreasing the secretion of renin, which leads to a decrease in total peripheral resistance. Adverse effects of b-blockers include bronchospasm, fatigue, impotence, hyperglycemia and altered lipid metabolism (Zamani et al 2007).
Centrally acting α2-adrenergic agonists such as methyldopa and clonidine reduce sympathetic outflow to the heart, blood vessels, and kidneys. Methyldopa is safe to use during pregnancy. Side effect includes dry mouth, sedation, and drowsiness is common; and in 20% of patients methyldopa causes a positive antiglobulin test, rarely haemolytic anaemia, and clonidine causes rebound hypertension if the drug is suddenly withdrawn (Neal M J 2009). Systemic a1-antagonists such as prazosin, terazosin, and doxazosin cause a decrease in total peripheral resistance through relaxation of vascular smooth muscle.
Calcium channel blockers (CCB) reduce the influx of Ca++ responsible for cardiac and smooth muscle contraction, thus reducing cardiac contractility and total peripheral resistance. Thus long-acting members of this group are frequently used to treat hypertension. There are two classes of CCB dihyropyridines and non- dihyropyridines. The main side effect of CCB is ankle oedema, but this can sometimes be offset by combining with β-blockers (Lip G YH 2003).
 Direct vasodilators such as Hydralazine and minoxidil lower BP by directly relaxing vascular smooth muscle of precapillary resistance vessels. However, this action can result in a reflex increase in heart rate, so combined β-blocker therapy is frequently necessary (Neal M J 2009). ACE inhibitors work by blocking the renin-angiotensin system thereby inhibiting the conversion of angiotensin I to angiotensin II.
Direct vasodilators such as Hydralazine and minoxidil lower BP by directly relaxing vascular smooth muscle of precapillary resistance vessels. However, this action can result in a reflex increase in heart rate, so combined β-blocker therapy is frequently necessary (Neal M J 2009). ACE inhibitors work by blocking the renin-angiotensin system thereby inhibiting the conversion of angiotensin I to angiotensin II.
ACE inhibitors may be most useful for treating patients with heart failure, as well as hypertensive patients who have diabetes. Using ACE inhibitors can lead to increased levels of bradikinin, which has the side effect of cough and the rare, but severe, complication of angioedema. A recent study demonstrated that captopril was as effective as traditional thaizides and β-blockers in preventing adverse outcomes in hypertension (Lip G YH 2003).
Angiotensin II antagonists act on the renin-angiotensin system and they block the action of angiotensin II at its peripheral receptors. They are well tolerated and very rarely cause any significant side-effects (Zamani et al 2007). Another helpful principle of antihypertensive drug therapy concerns the use of multiple drugs. The effects of one drug, acting at one physiologic control point, can be defeated by a natural compensatory mechanism (e.g. diuretic decrease oedema occurring secondary to treatment with a CCB).
 By using two drugs with different mechanisms of action, it is more likely that BP and its complication are controlled and the low dose range of combined drugs also help to reduce the side effects as well (Frank 2008). The following two-drug combinations have been found to be effective and well-tolerated diuretic and β-blocker; diuretic and ACE inhibitor or angiotensin receptor antagonist; CCB (dihydropyridine) and β-blocker; CCB and ACE inhibitor or angiotensin receptor antagonist; CCB and b-diuretic; α-blocker and β-blocker and other combinations (e.g. with central agents, including α2-adrenoreceptor agonists and imidazoline- I2 receptor modulators, or between ACE inhibitors and angiotensin receptor antagonists) can be used (ESH and ESC 2003).
By using two drugs with different mechanisms of action, it is more likely that BP and its complication are controlled and the low dose range of combined drugs also help to reduce the side effects as well (Frank 2008). The following two-drug combinations have been found to be effective and well-tolerated diuretic and β-blocker; diuretic and ACE inhibitor or angiotensin receptor antagonist; CCB (dihydropyridine) and β-blocker; CCB and ACE inhibitor or angiotensin receptor antagonist; CCB and b-diuretic; α-blocker and β-blocker and other combinations (e.g. with central agents, including α2-adrenoreceptor agonists and imidazoline- I2 receptor modulators, or between ACE inhibitors and angiotensin receptor antagonists) can be used (ESH and ESC 2003).
If necessary, three or four drugs may be required in many cases for the treatment. The use of a single drug will lower the BP satisfactorily in up to 80% of patients with hypertension but combining two types of drugs will lower BP by about 90%. If the diastolic pressure is above 130 mmHg then a hypertensive emergency occurs. Although it is desirable to reduce the diastolic pressure below 120 mmHg within 24 hours in accelerated hypertension, it is usually unnecessary to reduce it more rapidly and indeed it may be dangerous to do so.
This is because the mechanisms that maintain cerebral blood flow at a constant level independent of peripheral BP are impaired in hypertension. However, it is important to reduce the BP quickly by giving intravenous drugs but caution should be taken to avoid cerebrovascular pressure inducing cerebral ischemia (Grahame-Smith and Aronson 2002).
Conclusion
In conclusion, hypertension emerges as an extremely important clinical problem because of its prevalence and potentially devastating consequences. The major classes of antihypertensive drugs: diuretics, β-blockers, CCB, ACE inhibitors, and angiotensin receptor antagonists, are suitable for the initiation and maintenance of antihypertensive therapy which helps in the reduction of cardiovascular morbidity and mortality.
Read More On
- The Health Inequalities Between Genders
- Gender perception: How media affects our perception of gender.
- HIV Reverse Transcriptase: Molecular Mechanisms of Inhibition and Resistance
- Psychological and Sociological Factors Influencing Patient Care
- Critical Care of Chronic Obstructive Pulmonary Disease Patient: Reflection paper.
Do not hesitate to contact our professionals if you need help with a similar assignment.